* Dedicated to Prof. Jacek Dutkiewicz, PhD, on his 70th birthday.
|
Abstract: A 40-year-old female farmer is described, with a rare coexistence of 4 different occupational diseases sharing one common cause: allergy to cow epithelium (Bos domesticus). First symptoms started after 6 years of working on the farm. The allergic diseases appeared in the following sequence: rhinitis, protein contact dermatitis, asthma, conjunctivitis, and finally contact urticaria. The time span between the first and the last allergic manifestation to develop was 9 years. By the time of examination, 4 shock organs (the upper and lower airway, conjunctivae and the skin) were involved. Skin prick tests with common aeroallergens, farm animals, pets, and agricultural dusts were all negative, total IgE was within normal range (90 kU/l). Intracutaneous test and bronchial provocation with cow epithelium allergens were both positive. Specific IgE was detected to cow dander (CAP class 3) but not to bovine serum albumin (CAP 0). A positive reaction to goat dander (i.c. positive, CAP 2) was interpreted as a cross reactivity, because the patient never had contact with goats. The article also reviews known sources of cow allergens and occupations at risk. Besides farmers and veterinary surgeons, also butchers, cheese makers, bakers, cooks, laboratory workers and even beauticians may be at risk for developing occupational allergy to cow allergens. Key words: occupational allergy, farmers, agriculture, cow allergens, allergic rhinitis, conjunctivitis, contact urticaria, protein contact dermatitis, asthma, multiorgan allergy. |
There are 15 cow allergens (Bos domesticus) known nowadays, inclusive 3 variations of the major allergen Bos d 2 [1]. Seven of these allergens are listed in the official IUIS Allergen Nomenclature [17]. In occupational medicine, the hair- and epidermis allergen Bos d 2 [27, 30, 53] is probably most relevant. Despite specific IgE-antibodies against cow allergens are present in 1.1 - 8.8% of all farmers [26, 38], allergic airways diseases caused by them are relatively rare [29]. Also contact urticaria and protein contact dermatitis to cow are reported on in case reports only [3, 23, 32]. In this report, a farmer is described, in whom type I allergy to cow epithelium led to occupational diseases of 4 different shock organs.
Patient's history and medical examination
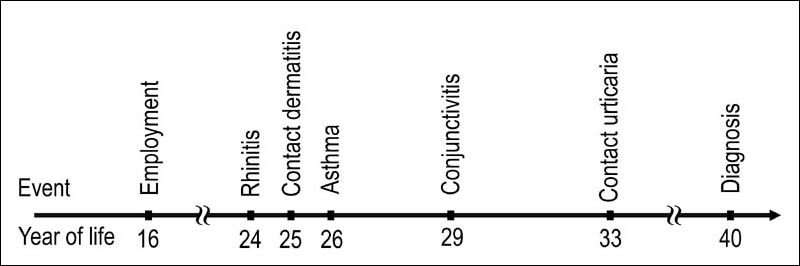
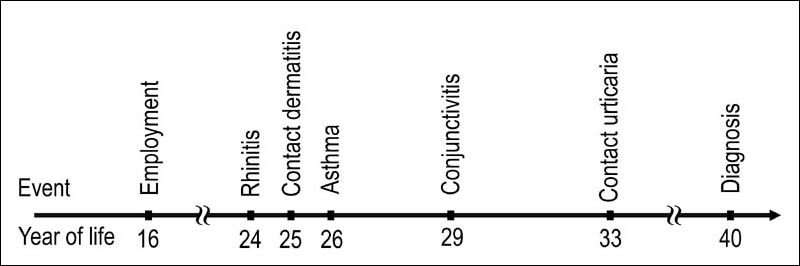
A 40-year-old female had worked on a family farm since the age of 16. After approximately 8 years of work, first symptoms appeared related to contact with cows (Fig. 1). Initially, these were attacks of sneezing with watery secretion. The symptoms appeared regularly after approx. 10 min after entering the cowshed and resolved half an hour after the end of the exposure. A year later, itching dermatitis emerged on the hands, predominantly in the interdigital spaces, caused exclusively by contact with cows. One more year later, the farmer had first episodes of dyspnea. Initially, shortness of breath appeared only while she was working with cows. Later, it was also caused by other activities. The main triggers of the dyspnea were the presence in cowsheds and physical effort. At the age of 29, the farmer suffered from a considerable aggravation of all the symptoms described above. Additionally, conjunctivitis was noted for the first time. Four years later, intensively itching wheals emerged on the skin areas exposed to contact with cows. The skin of the hands and forearms was most frequently involved. Occasionally also the forehead was involved when the patient leaned it against the cow's body during milking. The hives appeared within a few minutes after the contact and resolved an hour later. The farmer complained also about rhinitis when exposed to grain dust. The symptoms appeared during milling grain and feeding the animals. The grain-related symptoms were, however, considered by the patient as a minor problem.
Fig. 1. Progression of the farmer's symptoms.
Allergological diagnosis
The first examination revealed obesity and arterial hypertension. No symptoms of the skin and the airways were present. On rhinoscopy, there was a medium hyperaemia and swelling of the nasal mucosa.
Prick tests included cow allergens, other animals' epithelia, danders and feathers, house dust- and storage mites, moulds, flours and bran (Allergopharma, Reinbek), hay-, straw-, and grain dust (Biomed, Cracow). All these test gave negative results. Intracutaneous tests with animal allergens (Allergopharma, Reinbek) gave positive reactions to cow epithelium (wheal diameter 22 mm after 20 min), goat epithelium (18 mm) and sheep wool (17 mm). During the test, on the neck and both forearms of the patient isolated wheals appeared, which resolved without treatment after approximately 2 hours. A few hours later, the patient reported itching of the hands. On the next day, there was erythema and small vesicopapules in the interdigital spaces of the hands, which resolved after a week (with the patient's agreement, no treatment was undertaken in order not to compromise the following bronchial provocation). Patch tests with the European standard series (Chemotechnique Diagnostics, Malmö) revealed a (+)-reaction [36] to nickel sulphate. The buffering capacity of the skin was in normal range. Total IgE (90 kU/l) also was in normal range (up to 120 kU/l). Testing for allergen-specific IgE (UniCAP 100, Pharmacia, Uppsala) gave the following results: cow dander (8.08 kU/l = CAP class 3), goat epithelium (1.55 kU/l = CAP class 2). Specific IgE against other animal allergens, including bovine serum albumin, were not detectable.
The bronchial provocation test was carried out in a single-blind manner, after exclusion of contraindications [12]. The provocation was done according the following scheme: spirometry - one deep breath from the nebulizer - spirometry immediately, after 10 min and 20 min - 10 breaths from nebulizer - spirometry immediately, after 10 min and 20 min - 10 more breaths from nebulizer - spirometry immediately and after 10 min, 20 min, 1 h and 6 h. The FEV1-decrease of 20% was considered as a positive provocation result [13]. On the first challenge, the patient inhaled physiological saline with the preservative phenol as a negative control (0.5 ml in nebulizer, water bath temperature 37°C). The maximal FEV1 fluctuation did not exceed the 20%-limit. The second provocation was carried out according to the same scheme with a 1:1000 dilution of the original cow allergen solution (5000 BU/ml, Allergopharma, Reinbek). The result was negative. After the subsequent challenge with 1:100 allergen solution, the FEV1 decreased exactly by 20%. Facing the "borderline" result and a good status of the patient, further challenge with the 1:10 solution was undertaken. This time, 20 min after the inhalation of the whole dosis, FEV1 decreased by 27%. The patient complained of a dyspnea, which resolved after 2 doses of a fenoterol spray.
The presented case is interesting because of the diversity of symptoms caused by one allergen. Four occupational diseases were diagnosed, with involvement of 4 shock organs: the upper airway, the lower airway, the conjunctivae, and the skin. Such "multi-organ" occupational diseases are rare. There is only one report on a similar constellation of symptoms in the course of occupational allergy to nickel [9]. A coexistence of occupational urticaria, angioedema, rhinoconjunctivitis and asthma war recently reported, however, the coexisting diseases were caused by various allergens [31]. 44 years ago, a disease triad: rhinitis, asthma, and urticaria due to cow allergens was described [35]. Somewhat more frequently one can encounter occupational diseases of two shock organs, e. g. dermatitis with asthma [33, 39] or contact urticaria with allergic rhinitis [40]. A coexistence of contact urticaria and protein contact dermatitis (either parallel or subsequently) is relatively common [2, 51].
| Occupational disease | Allergen source | Occupations at risk |
|---|---|---|
| Rhinoconjunctivitis | Epithelia/Dander | Farmers [30, 41, 45, 48, this report]
Veterinarians [35] |
| Urine | Farmers [30, 48] | |
| Crystallised serum | Laboratory technicians [18] | |
| Bovine immunoglobulin G | Laboratory technicians [44] | |
| Asthma | Epithelia/Dander | Farmers [33, 45, 48, 52, this report]
Veterinarians [35] |
| Urine | Farmers [48, 52] | |
| Bone dust | Butchers [7] | |
| Crystallised serum | Laboratory technicians [18] | |
| Protein contact dermatitis | Epithelia/Dander | Farmers [8, 21, 23, 33, 35, 37, 41, 46, this report]
Veterinarians [15, 28] |
| Milk | Cheese makers [24, 35]
Farmers [37] |
|
| Saliva | Farmers [4] | |
| Amniotic fluid | Veterinarians [5, 15, 28, 32] | |
| Placenta | Beauticians [49] | |
| Blood | Butchers [54]
Veterinarians [5] |
|
| Meat | Butchers [3, 25, 54]
Cooks [16] |
|
| Intestines | Butchers [11] | |
| Liver | Butchers [10] | |
| Contact urticaria | Epithelia | Farmers [22, this report]
Veterinarians [35] |
| Amniotic fluid | Veterinarians [20, 34] | |
| Placenta | Veterinarians [34] | |
| Blood | Butchers [14] | |
| Serum | Veterinarians [20] | |
| Meat | Food handlers [50]
Bakers [19] |
In most European countries occupational allergy to cows is infrequent, despite the relative frequency of specific IgE in exposed groups [26, 29]. In a random sample of 68 Polish farmers (median age 47 years), the author found specific IgE to cow allergens in 8.8% and positive prick tests in 7.3%. None of the examined farmers complained of any health problems related to work with cows [38]. Among Polish farming apprentices (median age 19 years, farmers' children 87.5%), the sensitivity rate was significantly lower: Only 1 of 136 examined apprentices (0.7%) was prick test-positive, none complained of symptoms caused by contact with cows [42]. This suggests that sensitisation to cow allergens becomes more frequent with age, though in most cases it remains asymptomatic. In contrast to Poland and most other European countries, in Finland cow allergens are the most common cause for occupational contact urticaria [22]. This has two possible reasons: Because of the cold climate in Finland cows are kept up to 9 months yearly indoors. Moreover, Finnish farmers shave their cows in order to make them "look more clean". Altogether, this leads to an excessive allergen exposure (Susitaival, personal communication). Finnish researchers have confirmed the relationship between allergen concentration in cowsheds and immune reactivity of the farmers [47, 48]. Stability of the major allergen Bos d 2 and its presence in farmers' homes additionally increases the exposure [6].
The symptoms of the farmer described in this report are most likely related to contact with cows. Besides the convincing history, also the results of skin tests, specific IgE detection and positive bronchial provocation support the diagnosis. Positive test results with goat allergens are probably due to cross-reactions, as the patient had never contact to goats. Cross-reactivity between cow-, goat-, sheep-, and deer allergens was shown in both molecular and clinical studies [27, 40, 43].
For personal use only. © Dustri Verlag.
| Contact Dr. Spiewak | Back to article list | Website's front page |